1601006088 LONG CASE
HT no: 1601006088 - LONG CASE
This is an online e logbook to discuss our patients deidentified health data shared after taking her/guardian's signed informed consent
Here we discuss our individual patient problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs
This E log also reflects my patient centre’s online learning portfolio and valuable inputs on the comment box is welcome.
CASE:
A 50 year old female who is farmer by occupation, resident of suryapet came with chief complaints of weakness in left upper and lower limbs since 4 days.
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 4 days ago then she had dizziness which was sudden in onset then she developed weakness in her left upper and lower limbs followed by fall. Weakness in the limbs was sudden in onset, rapidly progressed to a state where she was unable to move her left side of the body. It was associated with drooping of angle of mouth on left side, with speech difficulty and there was deviation along with drooling of saliva from the angle of mouth when she attempted to speak
It was not associated with loss of consciousness, loss of memory, seizure activity, behavioral abnormalities, bowel or bladder incontinence or visual disturbances.
There was no history of fever, nausea, vomiting, headache, chest pain and dyspnea.
PAST HISTORY:
No similar complaints in the past
She is a known case of Diabetes and hypertension since 4 years which is under control by medication
No history of Tuberculosis, asthma, epilepsy, thyroid disease, cardiovascular disease.
FAMILY HISTORY: No relevant family history
MENSTURAL AND OBSTETRIC HISTORY:
She had underwent hysterectomy 4 years back for fibroid uterus.
PERSONAL HISTORY:
Diet - Mixed
Appetite - Regular
Sleep - Adequate
Bowel and bladder movements - regular
No addictions
ALLERGIC HISTORY:
No known allergic history
GENERAL EXAMINATION:
Consent obtained
Patient was conscious, coherent and cooperative, well built and well nourished
No Pallor, Icterus, Cyanosis, Clubbing, Koilonychia, General lymphadenopathy and Edema
VITALS:
Pulse : 75 bpm with regular rhythm and character
Respiratory rate : 15 cycles per minute
Blood pressure : 110/80 mm of Hg
Temperature : Afebrile
SYSTEMIC EXAMINATION :
Central nervous system :
Higher mental function:
Patient is consciousness, oriented to time place and person, emotionally stable, no loss of memory without behavioral abnormalities, speech is normal
Cranial nerves:
RIGHT LEFT
Olfactory nerve Intact Intact
Optic nerve Intact Intact
Occulomotor,
Abducense, Intact Intact
Trochlear nerve
Trigeminal nerve Intact Intact
Facial nerve
i) motor
Nasolabial fold Present Absent
Frowning Present Present
Closure of eyes Present Present
Whistling Present Absent
ii) sensory
Anterior 2/3rd of Present Present
tongue
iii) reflexes
Corneal Present Present
Conjunctival Present Present
Vestibulocochlear nerve Intact Intact
Glossopharyngeal, vagus Intact Intact
Spinal accessory Intact Intact
Hypoglossal nerve Intact Intact
Motor system:
RIGHT LEFT
Bulk No wasting No wasting
Tone
Upper limb Normal Hypotonia
Lower limb Normal Hypotonia
Power
Upper limb 5/5 0/5
Lower limb 5/5 4/5
Superficial reflexes
Corneal Present Present
Conjunctival Present Present
Plantar Flexor Extensor
Deep reflexes
Biceps +2 +2
Triceps +2 +2
Knee +2 +2
Ankle not elicited not elicited
Sensory system :
Superficial - Temperature, fine touch, pain are present
Deep - Positiom, Vibration, two point discrimination, Stereognosis, Graphaesthesia present
Cerebellar function - Normal
Coordination - Finger nose test, heel knee test present
Gait - Normal
Rombergs - negative
Signs of Meningeal irritation - Absent
OTHER SYSTEMS
CVS - S1, S2 heard
Respiratory system - Bilateral air entry present, vesicular breath sounds heard
Per abdomen - Bowel sounds heard
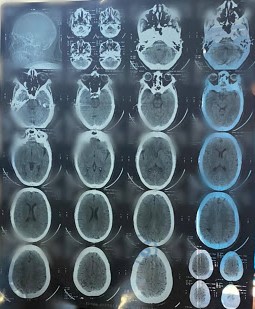
INVESTIGATIONS
CT Scan
ECG - Normal
PROVISIONAL DIAGNOSIS : Left UMN Facial Palsy with Left sided Hemiparesis







Comments
Post a Comment