1601006174 LONG CASE
1601006174 LONG CASE
Long case presentation
Consent is taken from patient and family members
A 45 year old male resident of Nalgonda who is a labourer by occupation presented with chief complaints of :
1)shortness of breath since 10 days
2)Cough since 9 days
3)Pedal edema since 9days
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 10 days ago,then developed
-Grade III shortness of breath which was insidious in onset ,non progressive,aggravated by walking and strenous work and dressing , relieved by sitting
-There is history of orthopnea
- There is no history of PND
-Dry Cough since 9days which is insidious in onset , non progressive ,no aggrevating and relieving factors
-Grade III bilateral Pedal edema since 9days which in insidious in onset , gradually progressive,pitting type , no aggravating and no relieving factors
-History of burning micturition and oliguria since 5 days
-There is no history of sweating , palpitations , chestpain , hematuria
PAST HISTORY:
- 2 years back he developed symptoms of productive cough and fever for 1 week for which he visited to hospital and diagnosed with TUBERCULOSIS and took antitubercular drugs for 6 months and at that time he was told be having some kidney issues and used some medications ( records notavailable )
-Not a known case of diabetes ,hypertension,asthma , convulsions
-Surgical history is not significant.
FAMILY HISTORY:
- Not significant
PERSONAL HISTORY:
-DIET : mixed
-APETTITE: normal
-Regular bowel habits
-Patient has oliguria and burning micturition
-He is an alcoholic since 10 years , drinks once weekly
-Smoker since 25 years , he smokes daily 2-5 beedis
GENERALEXAMINATION:
Patient is conscious coherent and cooperative , moderately built , moderately nourished
-Presence of pallor
-No icterus , no cyanosis, no clubbing ,no pedal edema
-No generalized lymphadenopathy
VITALS
-Pulse taken in sitting position ,left radial pulse ,Pulse rate : 80bpm , regularly regular
-Bp 130/80 mm Hgmeasured in sitting position on right upper arm
-Respiratory rate : 20cpm
-Afebrile
RESPIRATORY SYSTEM EXAMINATION:
Patient is examined in supine a well as in sitting positions under well ventilated room with consent taken
UPPER RESPIRATORY TRACT:
- Nose , oral cavity are examined and no abnormal findings are present
EXAMINATION OF CHEST PROPER:
Inspection:
-shape of chest : normal
-Symmetry of chest : symmetrical
-Trial sign negative
-Movements of chest :equal on both sides
RR -20cpm
-Type - abdomino thoracic
- No involvement of accessory muscles and no intercoastal tenderness
-No visible scars , no sinuses , no engorged veins
-No deformities of spine
-No visible apical impulse
Palpation:
-No tenderness and no local rise of temperature -Inspectory findings are confirmed
-Trachea central
-Apex beat : felt at 5 th Intercoastal space medial to mid clavicular line
-Decreased chest expansion
-Vocal fremitus : decreased at infra axillary and infra scapular areas on both sides normal on supra clavicular , infraclavicular ,mammary , infra mammary , suprascapular and interscapular areas
Percussion:
Direct percussion: resonant on clavicle , sternum
Indirect percussion :
Anterior :
-Resonant in supra clavicular area
-Resonant in infraclavicular area
-Resonant in inframammary area on both sides
-Traube’s space:dull
Posterior :
-Resonant in suprascapular area
-Resonant in interscapular area
-Dull in Infrascapular area on both sides
Auscultation:
-Bilateral air entry present
-Normal vesicular breath sounds heard
-Reduced in B/ L infrascapular and infra axillary areas
-Fine crepts heard on B/L infra axillary and infra scapular areas
CVS EXAMINATION:
-S1,S2 heard
-No murmurs
-No palpable thrills
ABDOMINAL EXAMINATION:
-Scaphoid shape
-No tenderness
-No palpable mass
-No hepatosplenomagaly
-No ascites
-Bowel sounds present
CNS EXAMINATION:
-Conscious and alert
-Normal gait
-Normal speech
-No signs of meningeal irritation
-Cranial nerves , motor system , sensory
-Reflexes : superficial and deep tendon reflexes are intact
INVESTIGATIONS:
-CBP
⁃CUE
-ABG
-RFT
-LFT
⁃PT
⁃APTT
⁃Blood sugar
-ESR
⁃Serum pottasium
⁃Blood culture
⁃Chest X ray
-ECG
⁃Ultrasound abdomen
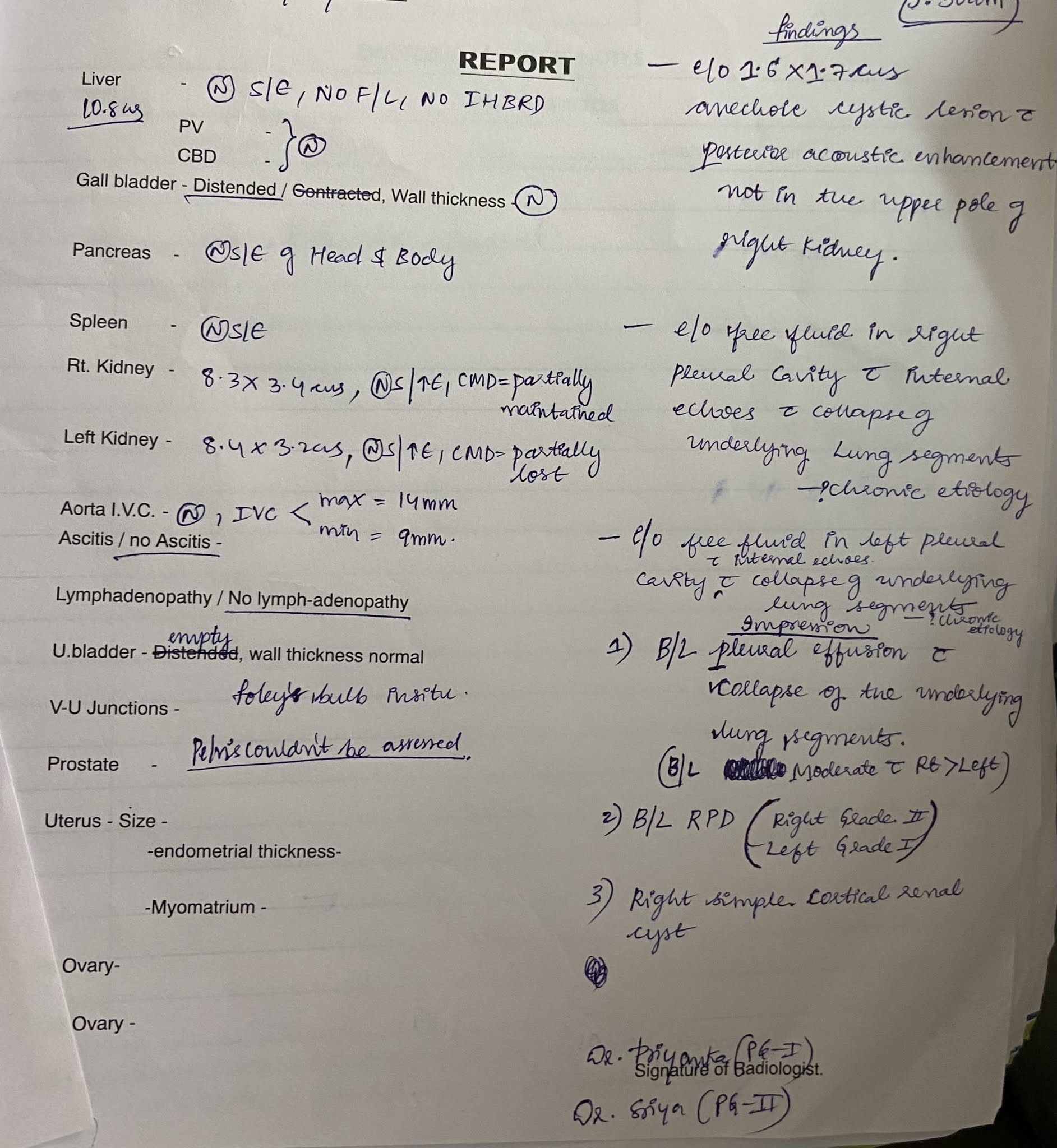
Provisional diagnosis :ACUTE ON CHRONIC RENAL FAILURE with pleural effusion with past history of pulmonary TUBERCULOSIS
TREATMENT:
-Salt and fluid restriction : Salt - < 2 g/ day ,Fluid - < 1 lt / day
⁃Injection iv LASIX 40mg BD
⁃Tab NODOSIS 500mg bd
⁃Tab SHELCAL 500mg od
⁃Input and output charting

















Comments
Post a Comment