1601006082 LONG CASE
1601006082 long case
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on
the comment box is welcome.
A 61 year old gentleman who is resident of Kangaal ,shepherd by occupation came with complaints of pain in abdomen from 10days,Fever from 2 days
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 10 days ago, then he developed
- Pain in abdomen - since 10 days which was insidious in onset, gradually progressive, diffuse, non radiating and dragging type of pain which was relieved while sleeping on his right side.No H/O diurnal variation.
- Fever - since 2 days which was a low grade, continuous fever associated with chills and rigor. It was relieved on taking medication.
- No History of nausea, vomiting, loose stools, flatulence, loss of weight, decreased urine output, dysuria.
PAST HISTORY:
- He had yellowish discolouration of eyes 6 months ago.
- No history of diabetes mellitus, hypertension, tuberculosis, epilepsy,asthma.
PERSONAL HISTORY:
- Mixed diet
- Appetite is normal
- Sleep adequate
- Bowel movements are irregular as he is constipated
- He is a chronic alcoholic takes 90ml/day since 30 yrs
- He is a chronic smoker and takes 20 beedis/day since 30 yrs.
FAMILY HISTORY: Not significant
TREATMENT HISTORY: Took medication in local hospital 6 months back for jaundice.
GENERAL EXAMINATION:
- Examination was done after taking proper consent & in a well lit room after adequate exposure.
- The patient is conscious, coherent and cooperative with well orientation to time, place and person
- He is moderately built and moderately nourished.
- Icterus is present in bulbar conjunctiva of both eyes
- Bipedal edema ,which is pitting type upto the level of ankle region


- There is no pallor, clubbing, cyanosis, koilonychia, generalised lymphadenopathy.
VITALS:
- Temperature - he is afebrile (at present)
- Pulse - 84 beats per minute, regular, normal in volume and character.
- Blood pressure = 120/70 mm of Hg in right arm in supine position
- Respiratory rate = 22 cycles per minute, abdominothoracic breathing
- Sp O2 :93% at room air
SYSTEMIC EXAMINATION:
A) GASTROINTESTINAL EXAMINATION:
1) Inspection:
a) Anterior abdominal wall
- Abdomen is symmetrically distended with full flanks
- Umblicus is below the midposition between xiphisternum and pubic symphysis, Slightly everted with horizontal Slit .
- Abdomen skin is smooth and shiny
- All the quadrants are equally moving with respiration
- No venous prominence when examined both on sitting and standing position.
- No scars ,ulcers ,visible pulsations.
- No Scratch marks on the abdomen.
- No hernial swellings with and without cough impulse
b) Posterior abdominal wall: No scars , swellings, pulsations
2) Palpation:
a) Superficial palpation:
- Localised tenderness in the right hypochondrium
- elastic consistency
- No rise in temperature, guarding and rigidity, thrills
- No palpable lymphnodes
b) Deep palpation,
- Liver is tender, smooth, firm, regular margin, moving with respiration.
- Spleen, kidneys, urinary bladder are not palpable
- Abdominal girth is 84 cms
3) Percussion:
- Liver span - 16 cms
- No shifting dullness .
- No fluid thrill
4) Auscultation,
- Bowel sounds are heard
- No venous hum,bruit, friction rub.
B) RESPIRATORY EXAMINATION:
1) Inspection:
- Upper respiratory tract examination - Brown staining on teeth, no deviated nasal septum, No nasal polyps, no post nasal drip
- Chest is symmetrical and elliptical in shape
- Trachea appears to be Central
- Movements of chest with respiration is equal on the both sides
- No Visible Pulsations, Swellings, Engroged Veins, Scars & Sinuses
- No signs of use of accessory muscles of respiration.
- No spinal deformities
2) Palpation:
- All the inspectery findings are verified
- No local rise of temperature
- Trachea Central
- Respiratory movements are normal
- Chest Expansion 5cm (from 80-85cm)
- Transverse diameter 29cm and AP diameter 24cm
- Vocal fermitus Decreased on Right side lower region
- Apex beat is palpable in 5th intercoastal space ,1 cm medial to mid clavicular line
- No palpable lymph Nodes
3) Percussion;
> Anterior chest wall
Right. Left.
- Supraclavicular Resonant. Resonant
- Infraclavicular Resonant. Resonant
- 2nd to 6th inter coastal spaces Resonant. Resonant
- 7th inter coastal space Stony dull. Resonant
> Lateral chest wall : Dull note in the right InfraAxillary region
> Posterior chest wall :
Right Left.
- Suprascapular Resonant. Resonant
- Interscapular Resonant. Resonant
- Infrascapular Dull Resonant
4) Auscultation:
Right. Left
- Supraclavicular Normal Normal
- Infraclavicular Normal Normal
- Mammary Normal Normal
- Inframammary Decreased Normal
- Infraaxillary Decreased Normal
- Suprascapular Normal Normal
- Interscapular Normal Normal
- Infrascapular Decreased Normal
C) Cardiovascular system examination:
- Normal S1 S2 heard
- No murmurs
- Apex beat felt on 5th intercostal space
D) Central Nervous system examination:
- No focal deficits seen
INVESTIGATIONS:
1) Complete blood picture
2) Complete urine examination
3) Liver function test:
4) Ultrasound Abdomen:
5) Aspiration of liver abscess:
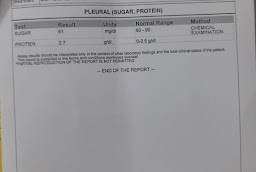
6) Pleural fluid examination:
7) Pleural tap:
8) Chest X-ray:
9) Abdominal X-ray:
TREATMENT:
1.INJ.MEROPENAM 500mg I.V ,BD
2.Inj.metrogyl 750mg I.V TID
3.Inj .pantop 40mg I.V,twice daily
4.Tab.Lasix 40 mg orally once daily
5 Tab.doxycycline 100mg oral twice daily
6.Tab.Linezoid 600mg per orally twice daily
7.Syrup lactulose 15 ml orally twice daily
8 Inj Vit.K 1 ampoule in 20ml .Normal saline I.V once daily
PROVISIONAL DIAGNOSIS:
Multiple pyogenic liver Abcess with right side pleural effusion.














Comments
Post a Comment