1601006070 LONG CASE
Final Exam Long Case
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs. This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment .
INTRODUCTION
40 year old male, labourer by occupation, resident of Narketpally came to OPD with chief complaints of
Breathlessness since 1 month
Fever since 10 days
Chest pain since 4 days
HISTORY OF PRESENTING ILLNESS
Patient was apparently asymptomatic 1 month back, then developed
breathlessness which was insidious onset which used to be grade 2(MMRC) and progressed to grade 4 since in the last 4 days with no postural or diurnal variation associated with generalised weakness. It was followed by low grade fever which was on and off since 10 days not associated with chills and rigor, shows no diurnal variation and relieved on medication, and
Cough since 7 days, associated with moderate amount of purulent sputum mixed with saliva which is whitish in colour with no postural variation and
Chest pain on left side on inspiration and coughing since 4 days which was non radiating and relieved on lying down.
No history of palpitation, syncopal attack, haemoptysis, recurrent sore throat, hoarseness, choking episode, joint pains, burning micturition, loose stools,constipation.
PAST HISTORY
Not a Known case of DM, hypertension, epilepsy, asthma, CVD, TB, thyroid disease
FAMILY HISTORY
No history of similar complaints in family.
PERSONAL HISTORY
Diet mixed
Appetite decreased
Sleep adequate
Chronic smoker since 14yrs 16-18 beedis/day
Chronic alcoholic since 10yrs and consumes 90ml/day.
Bladder and bowel movements are regular
GENERAL EXAMINATION
Consent obtained
The patient was examined in supine and sitting position.
Patient is conscious coherent cooperative well oriented to time place and person, has generalised wasting of muscles and is comfortable on bed.
There is no pallor, icterus, cyanosis koilonychias, clubbing, lymphadenopathy, pedal edema
JVP is not elevated, hepatojuglular reflex absent.
VITALS
Temperature : Afebrile,98 F
Respiratory rate : 40 cycles per minute
Pulse rate : 100 beats/min regular in rhythm character volume
Blood pressure : 90/70 mmHg left arm in sitting position.
Spo2 : 98% on room air.
SYSTEMIC EXAMINATION
Respiratory system:
1. Upper airway
Nose normal alae Nasi, septum
Oral cavity teeth pharynx normal no sinus tenderness
2. Examination of chest
INSPECTION
Shape of chest is flat
Both the shoulders appear to be at the same level
Trachea appears to be central
Apical impulse is not visible
Skin over chest is normal
Trail sign is absent
Hollownesss in supraclavicular and infra clavicular fossae
Movements of respiration:
Tachypnea is present and abdomino thoracic respiration
PALPATION
- No local rise of temperature
- No tenderness
- Chest is expanding equally on both sides
- Tactile vocal fremitus is increased infra axillary, infra scapular areas left side
PERCUSSION
Direct percussion on clavicle, sternum and Manubrium is resonant
Kronig isthmus resonant both sides
Indirect percussion(left) anteriorly mid claviclular line 2-6 intercostal spaces are resonant. Laterally mid axillary line 4-6 intercostal spaces are resonant, 5-7 intercostal spaces dull, posterity 9th intercostal space dull
Traube space is dull.
Indirect percussion(right) anteriorly mid claviclular line 2-6 intercostal spaces are resonant. Laterally mid axillary line 4-7 intercostal spaces are resonant. Posterity 9th intercostal space resonant.
AUSCULTATION
Left side infra clavicular, mammary, supra scapular, normal vesicular breath sounds, decreased bronchial breath sounds at infra axillary, scapular, infra scapular areas.
Crepitations at infra scapular area
Vocal resonance increased
Right side infra clavicular, mammary, supra scapular, infra axillary, infra scapular areas-vesicular breath sounds
Other system examination
CNS - no facial asymmetry all reflexes are normal
CVS- S1 S2 heard no added murmurs
ABDOMEN - abdomen is scaphoid with no organomegaly
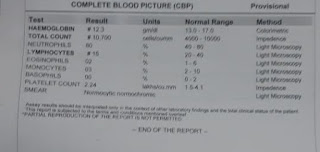
INVESTIGATIONS:
GRBS 650 mg/dl














Comments
Post a Comment